Based on typical use, Intrauterine devices (IUDs) have a failure rate of 0.8% per year, while the most popular birth control pill that requires daily dosing has up to 9% of failure rate. IUDs are also 90 times more effective than male condoms.
How various IUDs work?
While we have yet to invent a tiny uterus camera that can confirm with 100% certainty that this is how they work, experts, based on their laboratory studies, agree that the most likely mechanism of action behind extremely low tubal pregnancy rate of IUDs has to be as follows:
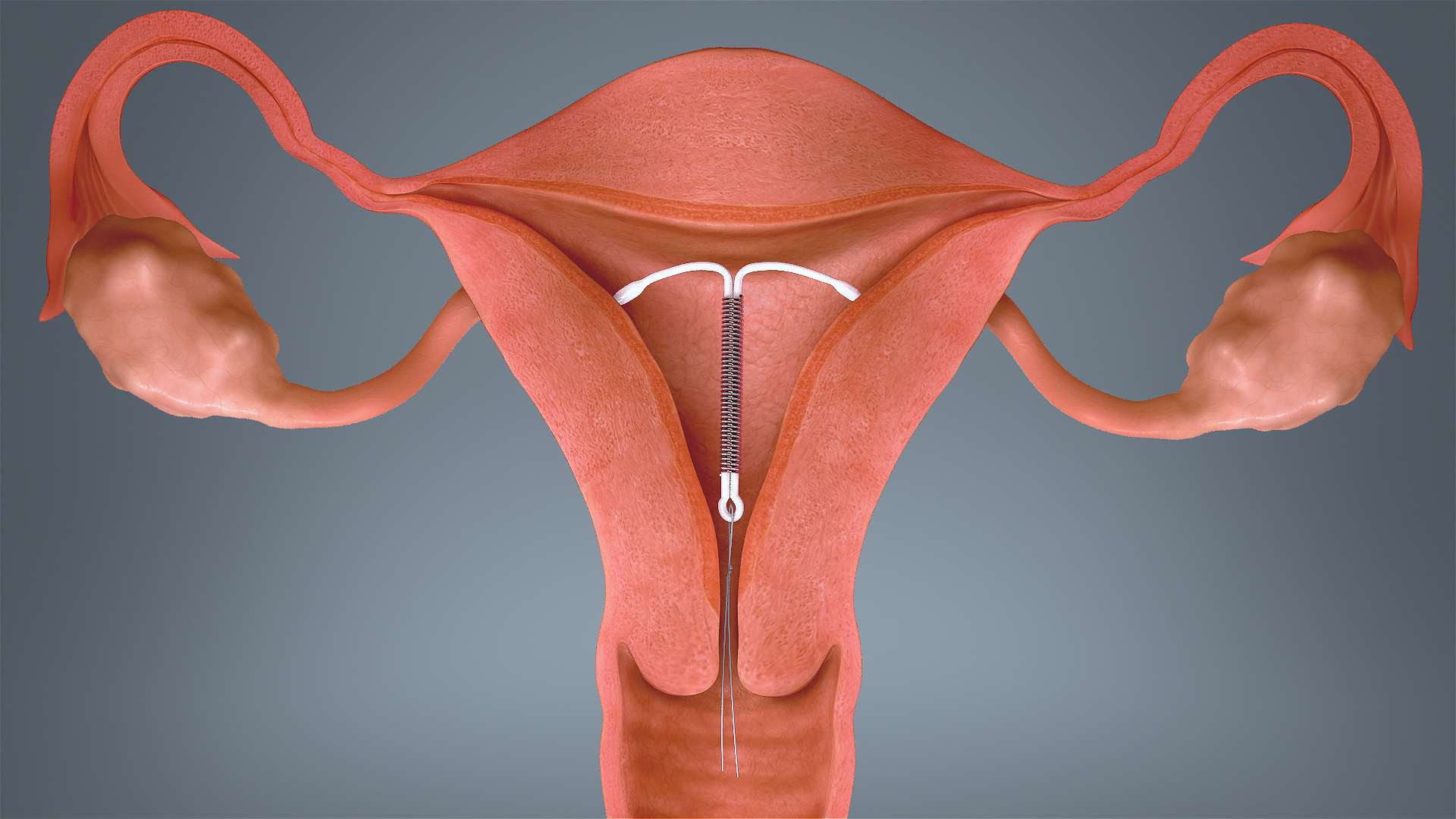
The 3 IUDs that are available in the US appear to work by blocking the sperm and egg from meeting (preventing conception). This is done by releasing hormones that thicken the cervical mucus, and prevent the sperm from swimming to the egg. The Paraguard is the hormone-free version (Copper T) that has copper coiled around its frame, causing a reaction in the body that makes the uterus toxic to sperm, thereby preventing fertilization.
Why fear?
The infamous Dalkon Shield IUD that was available in the 1970’s has to be blamed for the skepticism among people today. It was manufactured with a faulty string that attracted bacteria into the pelvis, leading to severe infections and even deaths. This faulty device created a negative bias against IUDs in the public as well as among the doctors who stopped prescribing IUDs. However, the bias is steadily beginning to overcome with quality research showing the safety and efficacy of the modern devices.
Contraception is certainly a personal decision, and shouldn’t be influenced by shallow opinions. But it is important to base the decision on medical facts, not on myths. This is why we’ve listed some common misconceptions to save you from getting influenced by wrong information you are likely to hear and believe.
MYTH 1: There’s a risk of infertility in young girls associated with IUDs
On the contrary, studies are showing a significant reduction in unplanned pregnancies with sexually active adolescents using IUDs vs birth control pills. Also IUDs have no effect on future fertility. The American Academy of Pediatrics and the American Congress of Obstetricians and Gynecologists, both recommend IUDs as the first line of defence for unwanted pregnancy owing to their incredible effectiveness.
MYTH 2: Inserting an IUD is painful
Pain-bearing capacity varies in different women. Every woman’s uterus, and experience, is unique. Some do experience significant pain with insertion, but that is not the norm. For most of them, the pain is short-lived and they get the device placed without any inconvenience.
MYTH 3: Your IUD could fall out
The uterus is intended to be an “exit only” organ so having a piece of plastic pushed into it is not the most fun procedure on the planet. However, there is only a 3 to 5% of chance that your body expels the IUD out from your uterus. That’s why doctors recommend that women use a backup contraception method for the first few weeks after the insertion.
MYTH 4: IUDs are dangerous and cause infections
Much like all medicines and medical devices, IUDs too come with some risks and complications. But the overall rate of complication is low compared to their satisfaction rate. Past 40 years of data shows that modern day IUDs are safe and don’t carry a high risk of infection. 1 out of 1000 insertions lead to uterine perforation, that too when the woman has just undergone a vaginal delivery and is still lactating.
Chances of infection exist only in the first month of insertion due to spread of preexisting cervical infections. This is why it’s recommended that patients be tested for sexually transmitted infections before insertion.
MYTH 5: Doctors have to induce a contraction to put the IUD inside the uterus
When putting an IUD, the doctor will open up your cervix slightly, first to measure your uterus, and then to insert the device. As both these movements stretch the cervix, they may cause a cramp sometimes that may last for 2-3 days. But a contraction is not induced through medicines as such.

Vasalgel: A male contraceptive to look forward to…
Effective reproductive control has always been dependent on female contraceptive methods, including daily pills and long-acting products such as IUDs and implants. Male contraceptive options available so far have been limited to condoms and withdrawal or vasectomy Read More..








