The two disruptive mental conditions which contribute to the ‘dysfunctionality’ of the normal human behavior, are intricately connected and often difficult to distinguish.
An individual diagnosed with a bipolar illness may develop the delusions and hallucinations usually associated with schizophrenia. Similarly, an individual diagnosed with schizophrenia can develop agitated states of mind that strongly resemble mania, and can also develop emotionally flat states of mind that bear some resemblance to depression. In fact, in any given person, the symptoms of the two disorders can overlap to such a degree that professionals in the field may have problems telling them apart, even after extensive observation and review.
Here’s a clear-cut list of features where schizophrenia and bipolar disorder strikingly overlap:
- Lifetime prevalence of about 1% in both males and females,
- Onset usually between late adolescence and early adulthood,
- Familial aggregation with very similar recurrence risks of the same disorder among relatives (~10-fold increase in children), and
- Comparable concordance rates for monozygotic and dizygotic twins with heritability estimates of 60-80%.
Since both these conditions are genetically complex with multiple genes operating in tandem with environmental factors, small changes in a large number of genes of an individual (some related to schizophrenia, some to bipolar, and some to both), can cumulatively increase the risk of developing one of the two psychotic ailments. This fact directly implies that certain abnormalities in the same set of genes may be shared by schizophrenia and bipolar disorder.
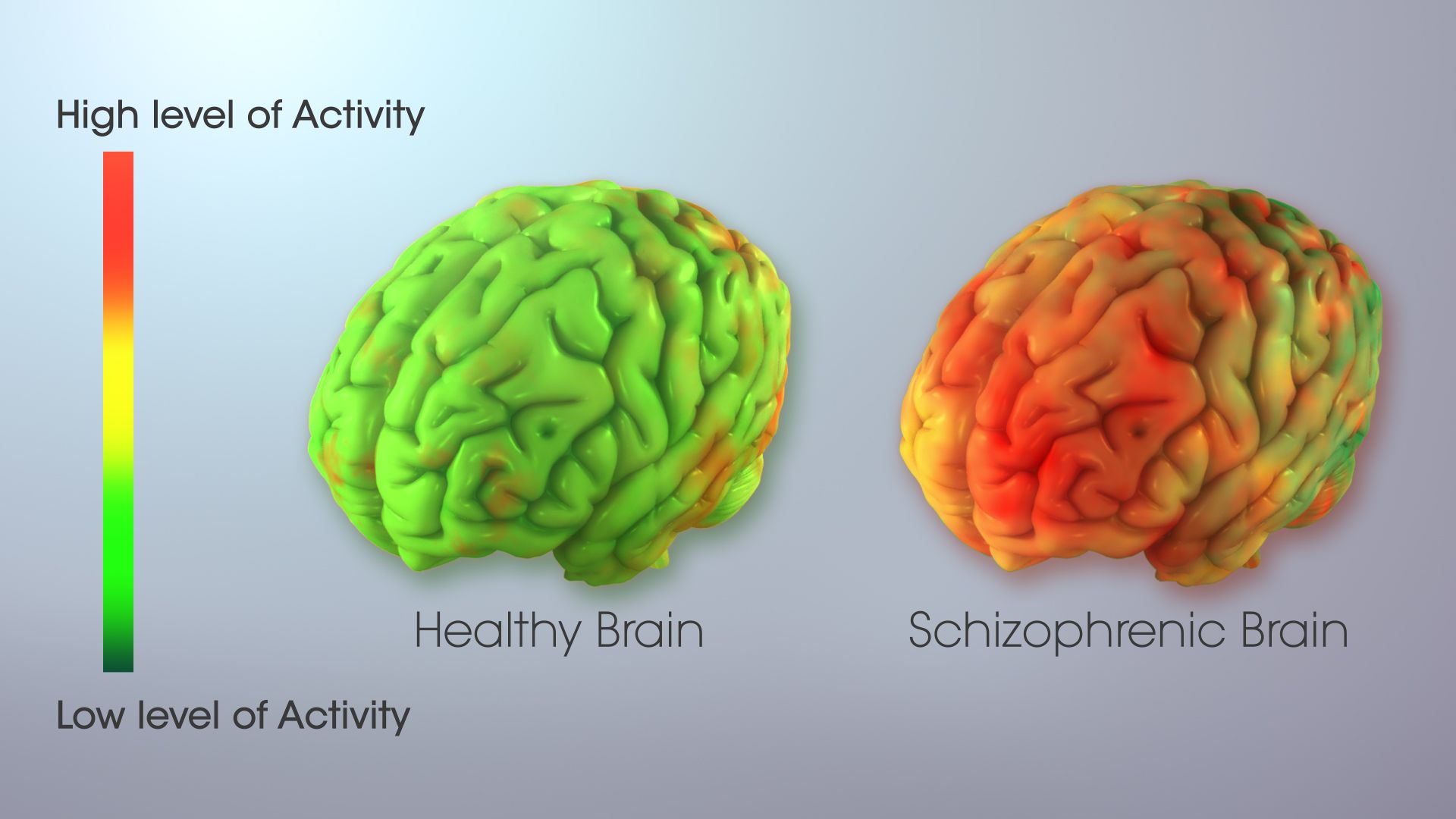
Further, both the conditions affect the same brain circuits (conscious mind), however, with varying intensity. Quite evidently, the malfunctions in the conscious brain in people with schizophrenia are more severe than those in people with bipolar illness. Because of this apparent distinction, the American Psychiatric Association officially places the two conditions in separate categories of mental illness.
The schizoaffective disorder classification is applied when an individual’s condition meets the diagnostic criteria for both schizophrenia and bipolar disorder. This makes the schizoaffective disorder the most challenging mental disorder to identify accurately and treat appropriately.
We will soon be releasing our next installment on Schizoaffective Disorder. Keep a check.
Eyes are the Windows to Mind: Early Detection of Alzheimer’s through Eye Tests
A fully manifested Alzheimer’s is marked by aggravated amyloid plaques and tangles that destroy the neurons and hamper the communication between them. However, unfortunately, the tangles and plaques are usually seen on autopsy after the patient’s death. Read More.....








