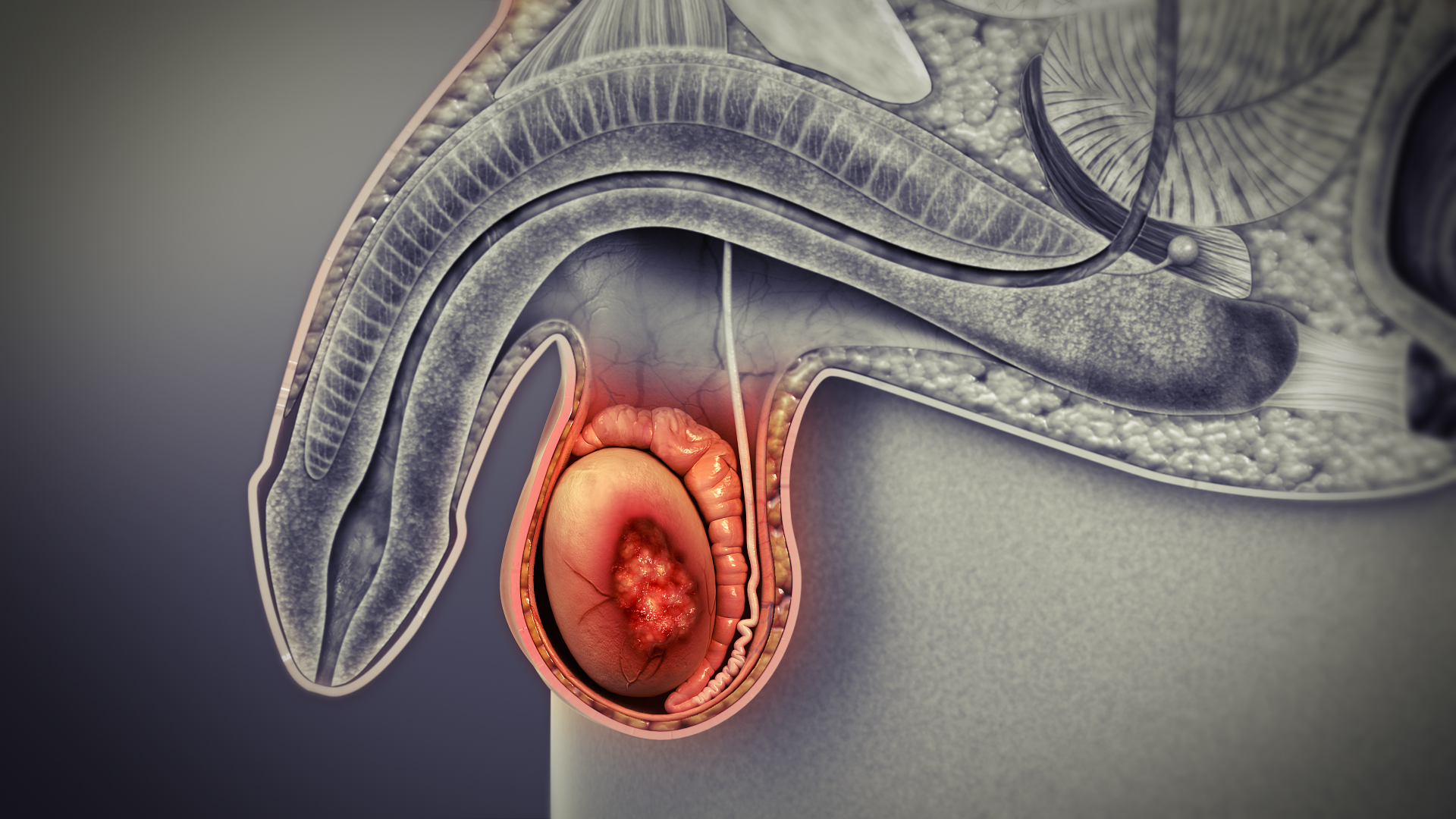
Testicular cancer, as is clear from the term, is a cancer that begins in the testicles of a male human being. The testicles are majorly responsible for the synthesis of androgens (male hormones) such as testosterone, and make sperms, male gametes needed to fertilize a female egg cell to start a pregnancy.
The word ‘cancer’ itself makes anyone cringe. But the fear and anxiety in this case can be at a little ease because...
The numbers are not that alarming, after all!
- As per the estimates provided by the American Cancer Society for the year 2017:
- About 8850* new cases of testicular cancer have been diagnosed.
- About 410 deaths have been reported from testicular cancer.
- With only about 1 of every 263 males developing it, testicular cancer is not common.
- Owing to the availability of successful treatment procedures, a man’s lifetime risk of dying from it is as low as 1 in 5000.
*The number had been rising at a fast rate, however lately, the rate of increase has slowed
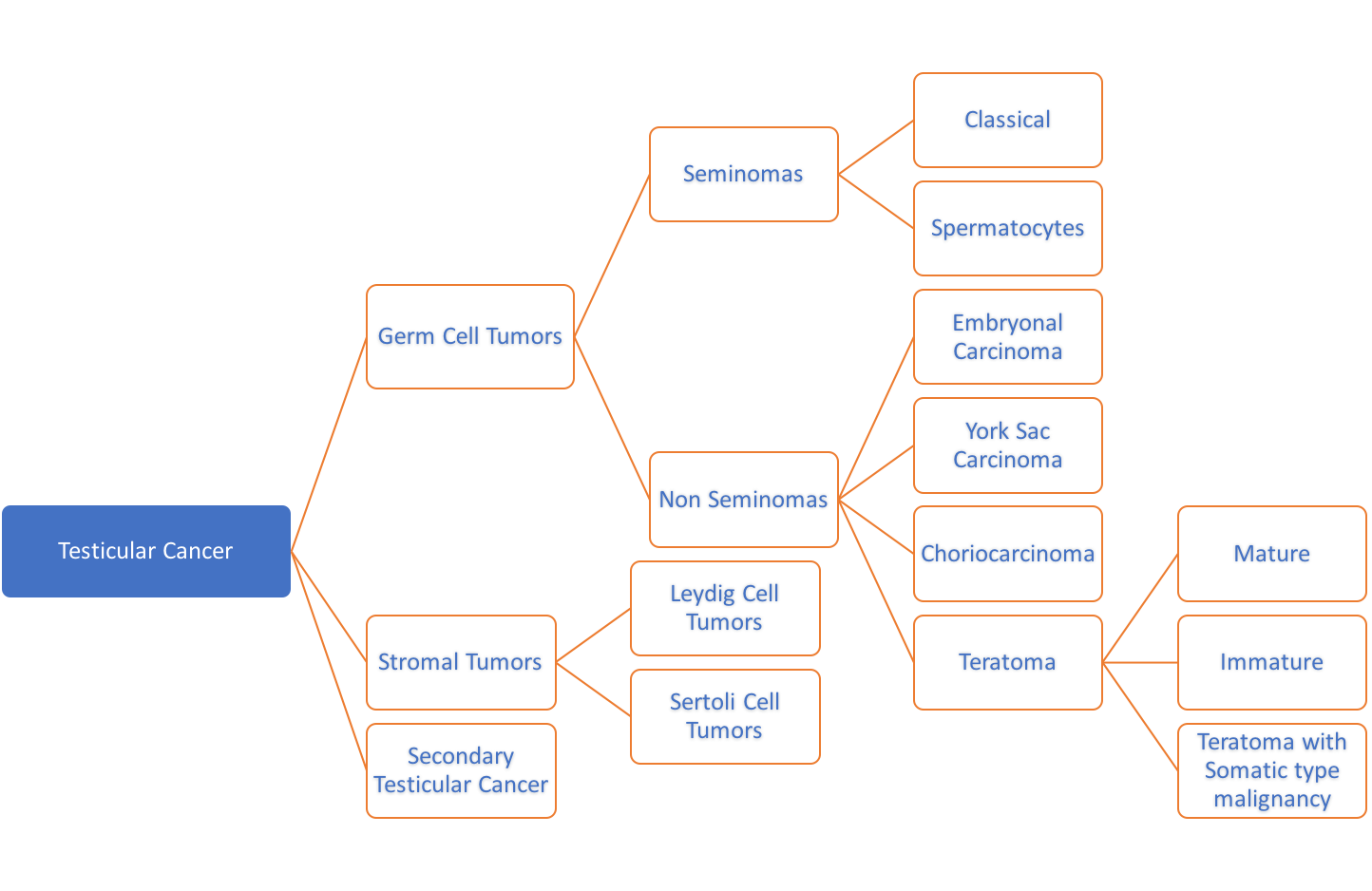
Testicular Cancer isn’t of a single type. It could manifest in several forms, each of which has a different process of being dealt with.
Several types of cells constitute the testicles. Cancer can develop in each of these, and hence, there are many types of testicular cancers. It is important to distinguish between these types because their prognosis and treatment would vary accordingly.
Germ cell tumors
This cancer is the most common and develops in the cells that make sperms (germ cells). The 2 main types of germ cell tumors in men are: Seminomas and non-seminomas. Non-seminomas are further made up of embryonal carcinoma, yolk sac carcinoma, choriocarcinoma, and/or teratoma.
Many testicular cancers contain both seminoma and non-seminoma cells. These mixed germ cell tumors are treated as non-seminomas because they grow and spread like that.
Seminomas grow and spread at a slower rate compared to non-seminomas. The 2 main subtypes of these tumors are classical seminomas (tend to occur in younger men) and spermatocytic seminomas (tend to occur in older men).
Moving to non-seminomas, the 4 main types are:
- Embryonal carcinoma: Under a microscope, these tumors can appear as tissues of very early embryos. This type of non-seminoma tends to grow rapidly and spread outside the testicle. Embryonal carcinoma can lead to increase in blood levels of alpha-fetoprotein (AFP), as well as human chorionic gonadotropin (HCG), so they can be used as tumor markers to detect and treat it.
- Yolk sac carcinoma: Also often referred to as endodermal sinus tumor, infantile embryonal carcinoma, or orchidoblastoma, these tumor cells resemble the yolk sac of an early human embryo. This is the most common form of testicular cancer in infants. When they occur in children, these tumors usually are treated successfully. But they are of more concern when they occur in adults, especially if they are pure. Yolk sac carcinomas respond very well to chemotherapy, even if they have spread. Yolk sac tumor almost always increases blood levels of AFP.
- Choriocarcinoma: This is a very rare and aggressive type of testicular cancer in adults. More often, choriocarcinoma cells are present with other types of non-seminoma cells in a mixed germ cell tumor. These mixed tumors tend to have a somewhat better outlook than pure choriocarcinomas. Pure choriocarcinoma spreads rapidly to distant organs of the body, including lungs, bones, and brain. This type of tumor increases blood levels of HCG (human chorionic gonadotropin).
- Teratoma: Teratoma tumors, under a microscope, look like each of the 3 layers of a developing embryo: endoderm, mesoderm, and ectoderm. Pure teratomas of the testicles are rare and do not affect AFP or HCG levels in the blood. More often, teratomas are seen as parts of mixed germ cell tumors.
The teratoma tumors formed by cells similar to those that constitute adult tissues, rarely spread to other parts of the body and are usually cured with surgery. These are known as Mature teratomas. Immature teratomas, on the other hand, are more likely to invade the surrounding tissues, to metastasize outside the testicle, and to recur years after treatment.
Teratomas with somatic type malignancy are very rare cancers. These cancers have some areas that look like mature teratomas but have other areas where the cells have become a type of cancer that normally develops outside the testicle (such as a sarcoma, adenocarcinoma, or even leukemia).
Stromal tumors
Stroma refers to the supportive, hormone-producing tissues of the testicles. The tumors that develop here are called gonadal stromal tumors. They make up less than 5% of adult testicular tumors but up to 20% of childhood testicular tumors. Most stromal tumors are benign and do not spread. However, stromal tumors that do spread sometimes do not respond to conventional treatments, like chemotherapy or radiation.
The 2 main types of stromal tumors are: Leydig cell tumors, that often make androgens (male hormones) but sometimes produce estrogens (female sex hormones), and Sertoli cell tumors that develop from sertoli cells that provide nourishment to the sperm-making germ cells.
Secondary testicular cancers
These cancers do not originate in the testicles, but rather migrate to it from other organs. The treatment of such cancers is, naturally, based on where they start. Secondary testicular cancers are, therefore, not true testicular cancers.
Let’s consider some examples:
- Lymphoma is the most common secondary testicular cancer. It occurs more often in older men than true testicular tumors. Depending on their type and what stage they are in, the prognosis varies. Lymphomas are usually removed surgically, followed by radiation and/or chemotherapy.
- Young boys who suffer with acute leukemia, often develop tumors in their testicles tumor in the testicle. Chemotherapy, alone, is not enough to cure it. Radiation therapy and surgery is also needed.
- Cancers originating in the prostate gland, lung, kidney, skin can also can spread to the testicles.