The SARS CoV-2 virus that causes COVID-19, has infected more than 36 million people and caused over 1 million deaths worldwide. Currently, neither the disease mechanism is known nor are there any treatments available. However, an emerging hypothesis on the possible Mechanism of Severe Disease -- which we’re calling the Bradykinin Hypothesis -- is one of the most compelling explanations of COVID-19 to date and could help evolve more therapeutic interventions to offset the severe effects of COVID-19.
An analysis was done on more than 40,000 genes from 17,000 genetic samples to better understand the disease. The results of the analysis revealed a new theory on how COVID-19 impacts the body - “the bradykinin hypothesis”. This hypothesis proposes that SARS-CoV-2 interferes in the regulation of bradykinin, a peptide that promotes inflammation and is responsible for vasodilation in the human body, which can explain many symptoms of COVID-19, including its less common ones.
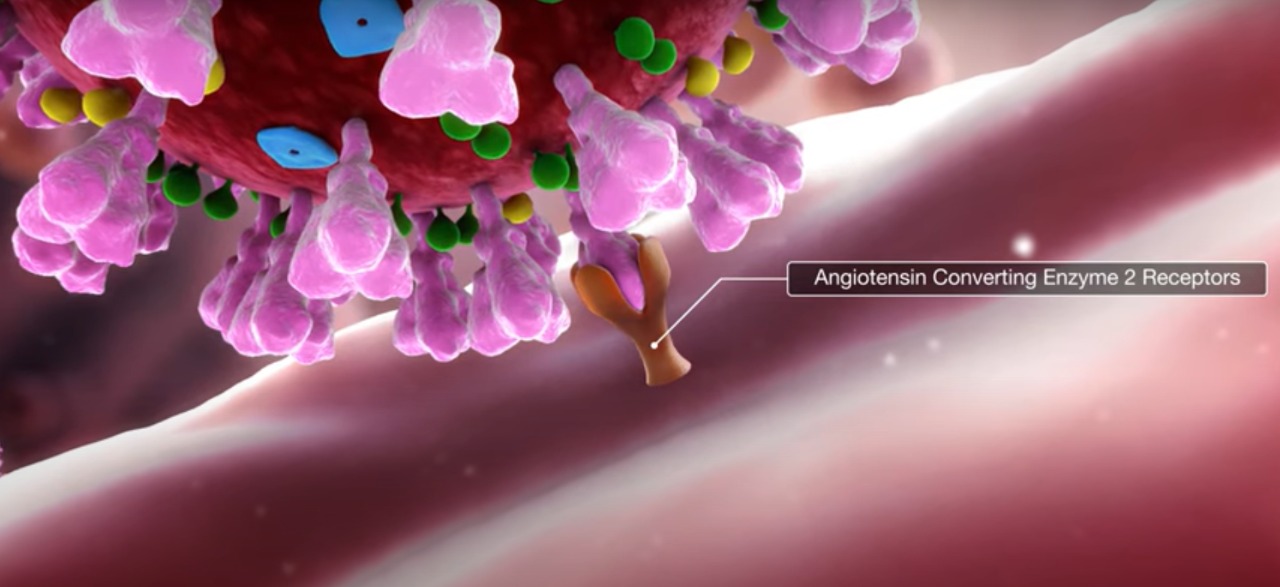
COVID-19 infection generally begins when the virus enters cells in the body through ACE2 receptors in the nose or respiratory tract; then the virus proceeds throughout the body, entering cells in other places where ACE2 receptors are present. ACE2 (Angiotensin-converting enzyme 2) lowers blood pressure in the body by breaking down angiotensin II, a vasoconstrictor peptide into angiotensin(1-7), a vasodilator. It counters the activity of another related enzyme ACE, which does the opposite work. So, the body has to balance the levels of ACE and ACE2 to maintain normal blood pressure. According to researchers, the virus doesn’t simply infect cells that already express lots of ACE2 receptors, instead it hijacks the body’s ACE2 regulatory mechanism and pushes the body to produce receptors where they’re less common, including the lungs.
The renin-angiotensin system (RAS) which is responsible for blood pressure regulation, and fluid and electrolyte balance in the body, controls the levels of bradykinin, which helps to regulate blood pressure. Normally, ACE breaks down bradykinin molecules, but when the virus downregulates it, it can’t do its work effectively. With decreased ACE activity, bradykinin levels are not controlled, and this leads to a bradykinin storm - a massive, uncontrolled buildup of bradykinin in the body. According to the hypothesis, the bradykinin storm is responsible for most of the deadly effects of COVID-19. As bradykinin builds up in the body, it increases blood vessels permeability and fluid and immune cells leak out of the vessels into the lungs. A byproduct of immune cells leaking out of the vessels is inflammation.
According to the data, the researchers said that the virus also increases the production of hyaluronic acid (HLA), in the lungs. HLA is a super absorbent, which is mostly used in soaps and lotions for its ability to absorb more than 1,000 times its weight in fluid. When it combines with the fluid leaking into the lungs, it results in the formation of a hydrogel in the alveoli that makes it difficult for patients to breathe, sometimes even with ventilator support. Bradykinin storms may also explain the cardiovascular conditions reported in some cases, even when the patient had no history of this. Some of this is likely due to the virus infecting the heart through ACE2 receptors. The bradykinin storms could also be the reason behind the cardiac arrhythmia and low blood pressure, which is mostly seen in COVID-19 cases.
According to the researchers, the bradykinin hypothesis also accounted for COVID-19 neurological effects which include dizziness, seizures, delirium, and stroke. Bradykinin, especially in high doses, can weaken the blood-brain barrier that protects the brain against damaging chemicals and cells (unregulated immune cells, etc). The weakening of the barrier could allow harmful cells and compounds into the brain, leading to inflammation, potential brain damage, and many of the neurological symptoms that are seen in COVID-19 patients.
The researchers said that increased levels of bradykinin could also account for other common COVID-19 symptoms. They noted that the virus has a similar effect to ACE inhibitors that are prescribed for controlling high blood pressure—ACE inhibitors are known to cause dry cough and fatigue, the two most common symptoms of COVID-19. ACE inhibitors can increase the potassium levels in the blood, which is also observed in COVID-19 patients. They are also known to cause a loss of taste and smell, however, the team says that this symptom is more likely due to the virus affecting the cells around olfactory nerve cells than the direct effects of bradykinin.
The team speculated that COVID toes, a condition involving swollen and bruised toes, which most of the COVID patients experience, could be due to the leaky vasculature caused by the Bradykinin storm. The Bradykinin can also interfere with the thyroid gland and result in the thyroid symptoms which are recently observed in some COVID patients.
The Bradykinin hypothesis also explained some of the demographic features of the disease. The researchers noted that some aspects of the RAS are sex-linked, with proteins for several receptors, located on the X chromosome. This means that women are more likely to have twice the levels of this protein than men, which could explain the lower incidence of COVID-19 induced mortality in women.
The team pointed out that several existing medicinal drugs such as danazol, stanozolol, and ecallantide reduce bradykinin production and can potentially stop the bradykinin storm. They also suggested that vitamin D as a potentially useful COVID-19 drug, as it is involved in the RAS system and could ultimately stop the formation of bradykinin storms. All of these potential treatments are speculative, and of course, need to be tested for their safety and efficacy before they could be used more broadly.
Disclaimer: The information in no way constitutes, or should be construed as medical advice. Nor is the above article an endorsement of any research findings discussed in the article an endorsement for any of the source publications.








