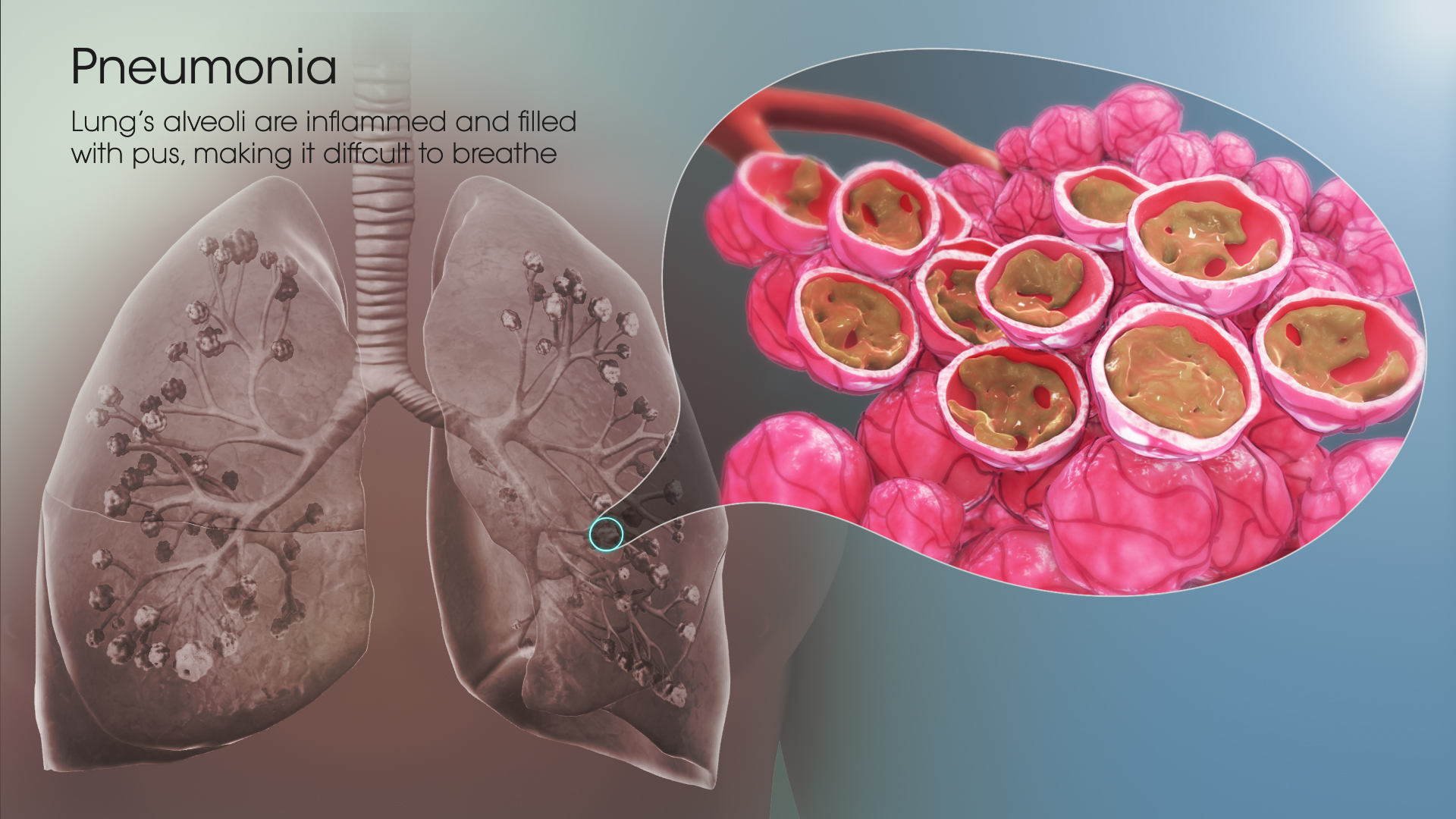
Pneumonia is an inflammatory condition of the lung (pneumonitis) and the leading cause of death of children under 5 years old worldwide. In the US, around 1 million people are hospitalized for pneumonia with 50,000 deaths per year. Those at high risk for pneumonia include the elderly, the very young, and people with underlying health problems.
Pneumonia is not a single illness but many different illnesses, each caused by a different microorganism.
Often, pneumonia starts as an upper respiratory tract infection and moves into the lower respiratory tract. The airways and lungs are constantly exposed to microscopic organisms. Microorganisms are always present near the nose and throat almost all the time, and people regularly inhale these organisms.
The flora of the upper airway competes with pathogens for nutrients, while in the lower airways, cough reflexes, actions of complement proteins and immunoglobulins, aid in expelling out the mucus and foreign substances.
The progression of pneumonia depends on the virulence of the causative organism, the organism load of the initial infection, and the body’s immune response to the infection.
Types of Pneumonia
Pneumonia is classified in different ways.
Healthcare professionals often refer to pneumonia based upon the way that the infection is acquired- community-acquired pneumonia or hospital-acquired pneumonia.
Community-acquired pneumonia (CAP) is more common than hospital-acquired pneumonia. It is most common in winter and affects about 4 million people a year in the U.S.
Hospital-acquired pneumonia (HAP) is acquired when an individual is already hospitalized for another condition. It is, hence, more serious. Being on a ventilator for respiratory support increases the risk of acquiring HAP.
Based on the way the inflammatory cells infiltrate the lung tissue or the appearance of the affected tissue, pneumonia can be:
Bronchopneumonia: Scattered, patchy infiltrates of inflammation in the air sacs throughout the lungs.
Lobar pneumonia: Inflammation of one lobe of a lung, typically involving all the airspaces.
Lipoid pneumonia: Aspiration of oils and fats in the airspaces that cause obstruction.
Sometimes, types of pneumonia are referred to by the type of organism that causes the inflammation- bacteria, virus or fungus. The specific organism name may also be used to describe the types of pneumonia, such as pneumococcal (Streptococcus pneumoniae) pneumonia or Legionella pneumonia.
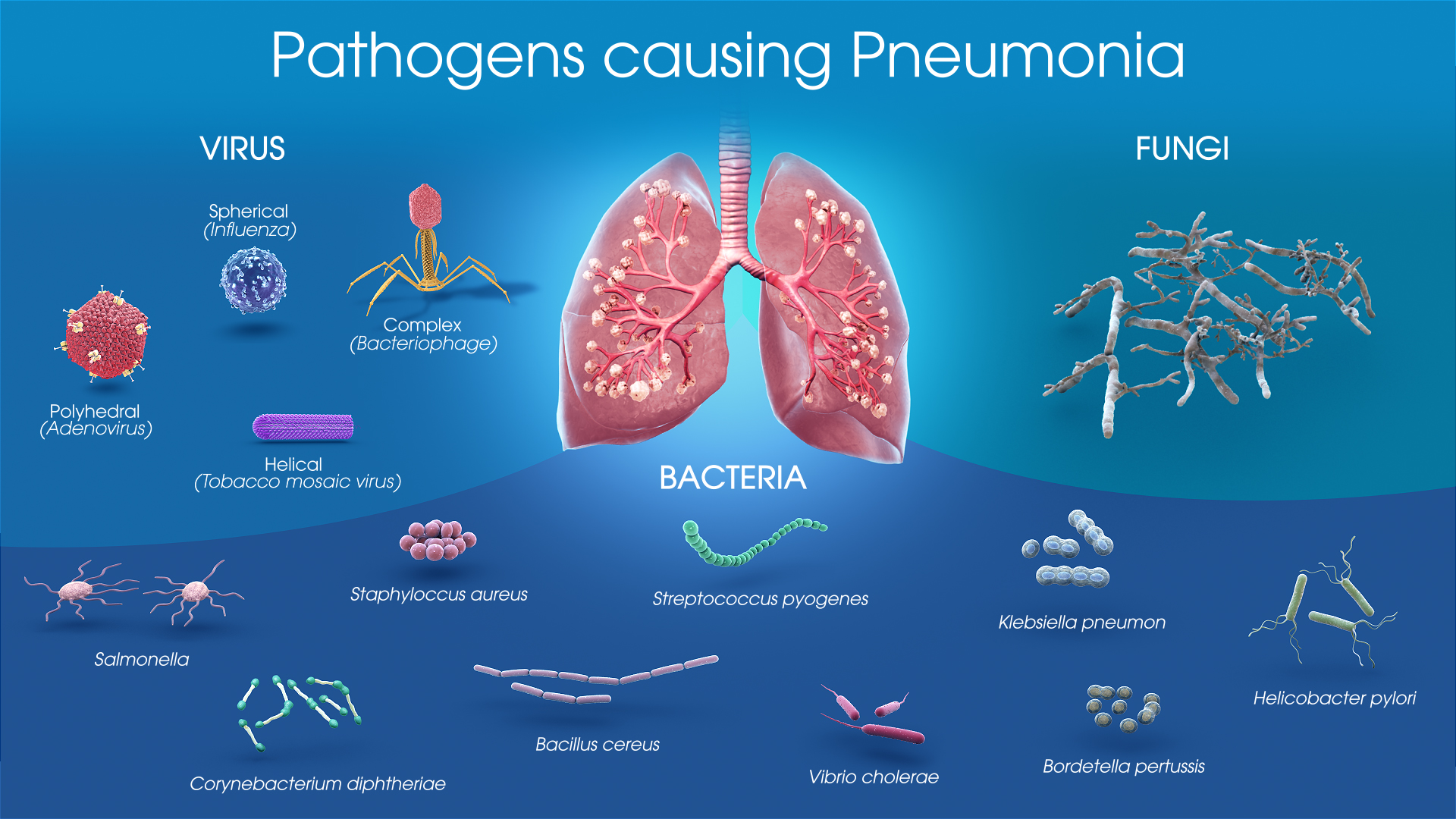
Viral pneumonia
Viruses may reach the lung by a number of different routes - touching contaminated objects and then their eyes or nose, or inhaling contaminated droplets in air. Once in the upper airway, they make their way into the lungs and invade the cells lining the airways and alveoli. The invasion of the lungs may lead to varying degrees of cell death. When the immune system responds to the infection, even more lung damage may occur, as white blood cells cause inflammation. Viruses also make the body more susceptible to bacterial infections; in this way, bacterial pneumonia can occur at the same time as viral pneumonia.
Bacterial pneumonia
Most bacteria enter the lungs via small aspirations of organisms residing in the throat or nose. Half of normal people have these small aspirations during sleep. While the throat always contains bacteria, potentially infectious ones reside there only at certain times and under certain conditions.
Bacteria such as Mycobacterium tuberculosis and Legionella pneumophila reach the lungs via contaminated airborne droplets. Bacteria can spread also via the blood.
Macrophages and neutrophils (defensive white blood cells) attempt to inactivate the bacteria. The neutrophils also release cytokines, causing a general activation of the immune system. This leads to the fever, chills, and fatigue common in bacterial pneumonia. The neutrophils, bacteria, and fluid from surrounding blood vessels fill the alveoli and this can be clearly observed in the patient’s chest X-ray. The most common cause is the bacterium Streptococcus pneumoniae, but many different bacteria can cause pneumonia.
Fungal pneumonia
It can result from a condition such as valley fever, caused by the Coccidioides fungus.
Other types of pneumonia are:
Aspiration pneumonia develops as a result of stomach contents (food or drink, saliva, or vomit) blocking the lungs. This occurs when the swallowing reflex is impaired, such as with brain injury or in an intoxicated person. Aspiration pneumonia, however, is not contagious.
Pneumonia caused by Legionella pneumophila, Mycoplasma pneumoniae, and Chlamydophila pneumoniae, is referred to as atypical pneumonia or sometimes "walking pneumonia" as it does not require bed-rest or hospitalization. This is because its symptoms differ from those of other types of bacterial pneumonia.
Pneumonia that arises from being on a ventilator for respiratory support in the intensive-care setting is known as ventilator-associated pneumonia.
Regardless of the cause, the signs and symptoms will be similar.
Treatment and Prevention
Vaccinating both adults and children prevents them from bacterial and viral pneumonias. Healthcare workers are also immunized to decrease their risk of contracting pneumonia from patients.
There are two different vaccines to prevent pneumococcal disease, the most common bacterial cause of pneumonia.
- Prevnar, a pneumococcal conjugate vaccine
- Pneumovax, a pneumococcal polysaccharide vaccine
Roughly one-third of all pneumonia cases in the US are caused by respiratory viruses, most commonly influenza.
Vaccinating children against Streptococcus pneumoniae has led to a decreased rate of these infections in adults, because many adults acquire infections from children. The CDC recommends that children (both young and old) and elderly adults (65+) to receive the pneumococcal vaccine, as well as older children or younger adults who have an increased risk of getting pneumococcal disease.
Medications
About 80% of cases of CAP can be managed at home with the patient taking oral antibiotics. The exact choice of medications depends on many factors, including the following:
- The causative organism
- The probability that the organism is resistant to certain antibiotics
- The patient's underlying health condition
Early antibiotic treatment is successful for most bacterial infections. Certain drugs can also effectively treat fungal pneumonia. However, medication is usually ineffective in treating the viral types of pneumonia.
Administering antibiotics to pregnant women having Streptococcus and Chlamydia trachomatis infection, reduces rates of pneumonia in infants. In the frail elderly good oral health care may lower the risk of aspiration pneumonia. Zinc supplementation in children 2 months to five years old appears to reduce rates of pneumonia.
Neuraminidase inhibitors may be used to treat viral pneumonia caused by influenza viruses (influenza A and influenza B). The use of antibiotics in viral pneumonia is recommended by some experts, as it is impossible to rule out a complicating bacterial infection.








