Urinary tract infections are infections of the urine-producing/carrying organs: kidneys, ureters, bladder and urethra. When the infection is confined to the bladder and urethra, this is called a lower UTI. If it travels up to affect one or both kidneys as well then it is called an upper UTI. This can be more serious than lower UTIs, as the kidneys can become damaged by the infection.
Women are more likely to develop UTIs in comparison to men, but, having said that, UTIs in men are typically more complicated.
UTIs are rare in young men; their risk increases post 50 years of age.
This could be due to the following reasons:
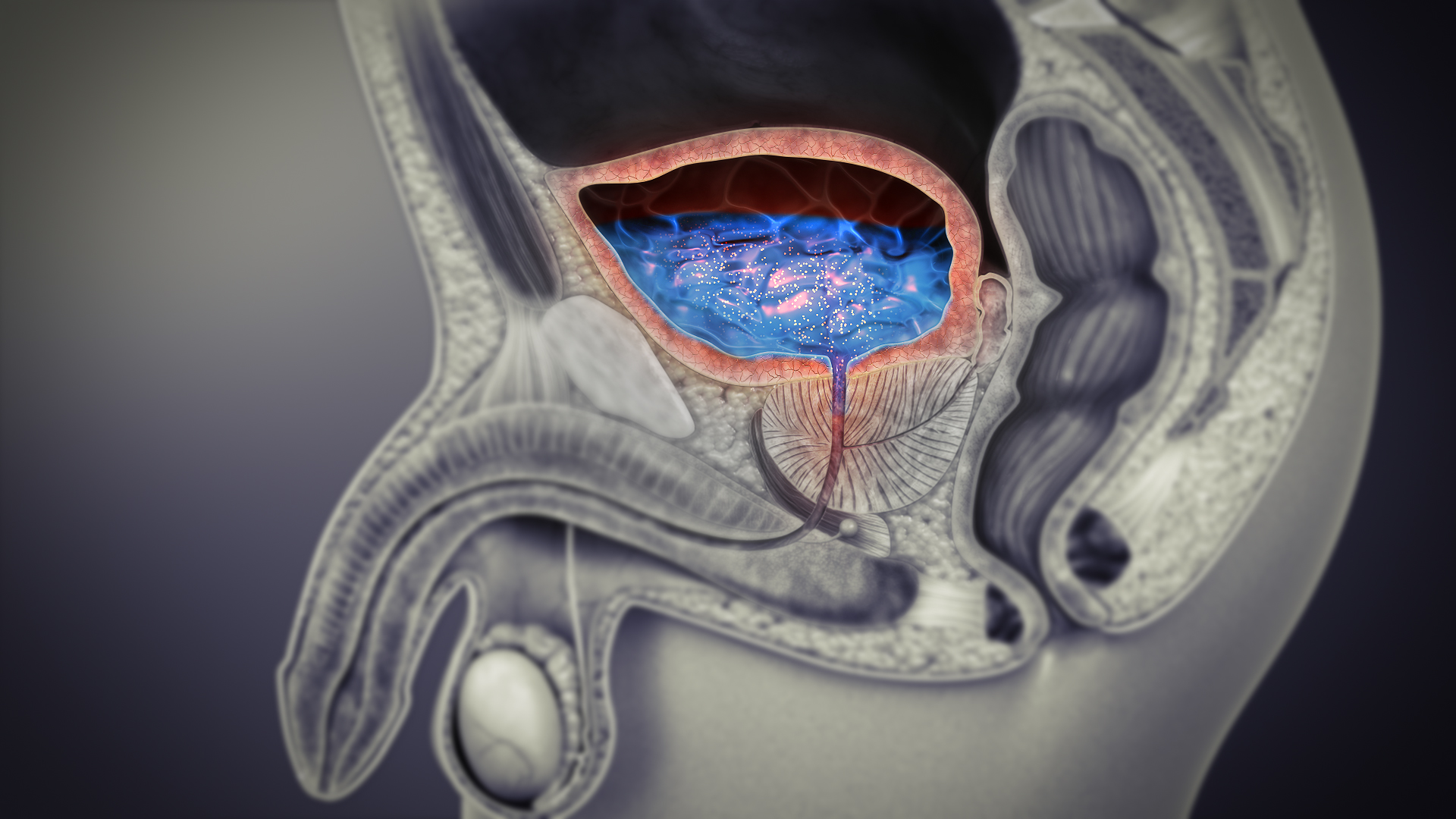
- Enlarged prostate: An enlarged prostate may prevent proper emptying of bladder. Some urine may then pool in the bladder, in which, the bacteria are more likely to multiply and cause infection.
- Kidney stones
- Diabetes
- Catheter insertion in the urinary bladder: A thin, flexible, hollow tube, passing from the bladder to the outside, is used to help pass urine in a number of different circumstances. Having a catheter is the most common cause of urine infections which develop in hospital.
- Any health condition that affects the immune system: .A poor immune system increases the risk of having any infection, including urine infections. For example, if you have AIDS or are taking chemotherapy.
Older males with prostatic hypertrophy have incomplete bladder emptying, predisposing them to UTI on the basis of urinary stasis.
Recognizing UTI in men- Some common signs:
- Constant urge to urinate
- Releasing only small amounts of urine at a time
- Cloudy-looking, foul-smelling urine, often with blood
- Abdominal or lower back pain
- Burning pain during urination
- Fluid seeping from the penis
Let’s talk in depth about each type of UTI that men are likely to face.
Pyelonephritis
Starting from the most serious, upper tract UTI that affects the kidneys. Pyelonephritis is an infection of the renal parenchyma. Infection usually occurs in ascending fashion (due to retrograde flow of bacteria) from the bladder. The ureteral orifice loses its one-way valve function during infection.
Virulent strains of S aureus are mostly the causative organisms of pyelonephritis. E coli is responsible for approximately 25% of cases in males, while Klebsiella, Pseudomonas, Serratia, and enterococci are less frequent. Endotoxin from gram-negative organisms can retard ureteral peristalsis.
Bacterial cystitis
Bacterial cystitis usually occurs as a concomitant infection with other parts of the genitourinary tract, or in association with an anatomic abnormality, defect in bladder emptying mechanism, or urethral catheterization. This is because high voiding pressures and poor bladder compliance diminish the natural uroepithelial resistance to infection and elevated post-void residuals allow bacteria to multiply to critical levels.
The symptoms are: irritative voiding of urine that can range from frequency, urgency, to pain sensation.
Urethritis
When N gonorrhoeae penetrates the urethral epithelium, it leads to periurethral pus accumulation. The term gonorrhea is a combination of ‘gonus’ meaning seed and ‘rhoia’ meaning flow.The dead epithelial cells collect as debris in the lumen of urethra, producing a milky penile discharge.
Gonococcal urethritis remains the most commonly reported communicable bacterial disease in the United States.
Prostatitis- Acute and Chronic
45 plus old males experience an increased level of adenomatous elements of the prostate, leading to its significant enlargement. This further causes obstruction in bladder outflow, hence, accumulation of residual urine.
Acute prostatitis infection of the entire prostate gland results in fever and localised pain. It is caused by uropathogens and responds promptly to antibiotic therapy.
Chronic prostatitis is a subacute infection which is characterised by recurrent UTIs. It may be caused by inflammatory or noninflammatory diseases.








