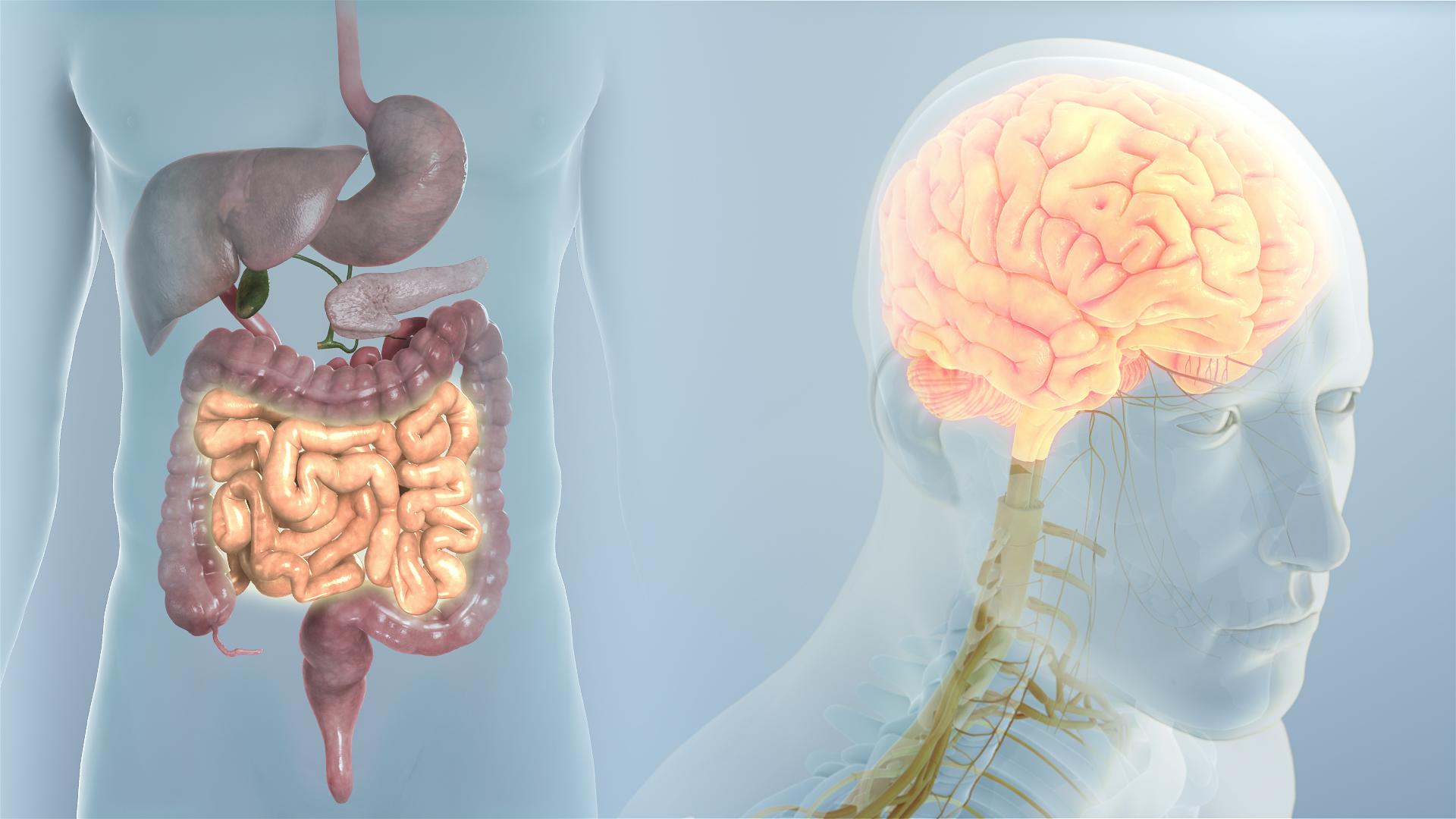
As the brain and the intestine are so close morphologically, they are also closely related and capable of influencing each other. Let’s find out how...
We already talked about how inflammatory infections originate in the gut. Seems like the gut also gives rise to neurodegenerative diseases.
According to a study published in Cell, the gut microbiota promote neuroinflammation and motor deficits in a mouse model of Parkinson’s disease.
Parkinson’s disease involves the death of neurons deep within the brain, causing tremors, stiffness and difficulty in movement. It was proposed that the nerve damage leading to Parkinson's starts in the stomach or colon before spreading to brain cells.
Remarkably, 70 percent of the neurons of the peripheral nervous system are in the intestines, and the nervous system of the gut is directly connected to the central nervous system through the vagus nerve.
Inflammation makes synuclein more likely to aggregate
A distinctive feature of Parkinson’s is the occurrence of synuclein (insoluble fibre like substance) deposits in the nerve cells. Synuclein molecules are normally found in traces and are soluble in healthy nerve cells, but in PD patients, they wrap into a different shape and get clumped together as fibers.
Pathologists, while performing autopsies of PD patients, had observed the presence of synuclein fibers in nerves of the gut. Some of the deceased didn’t even show the symptoms of the condition during their lifetime but only had the fibers in their brain.
It is now believed that there is a mechanistic link between the disease and the production of short-chain fatty acids by gut microbiota. The bacteria can break down fiber into short-chain fatty acids. It is thought an imbalance in these chemicals triggers the immune cells in the brain to cause damage. The brain-gut interactions are significantly modulated by the gut microbiota via immunological, neuroendocrine, and direct neural mechanisms. Dysregulation of the brain-gut-microbiota axis in PD may be associated with gastrointestinal manifestations frequently preceding motor symptoms, as well as with the pathogenesis of PD itself, supporting the hypothesis that the pathological process is spread from the gut to the brain.
The discovery seems sensible because PD patients often complain of constipation and other digestive problems much much before they notice tremors which are said to be the ‘real’ symptoms.
If changes in the microbiome may be involved in Parkinson's disease, this will potentially open novel and effective possibilities for treatment.
Parkinson's is currently incurable. So if these findings get confirmed, probiotics and drugs that work in the digestive system may become new therapies for the disease.
Graphene: Our Brain’s New Friend
Neural implants are of great value in neuroscience research as they enable a connection between nervous tissue and the ex vivo environment. Because of this, they also provide therapy for patients oppressed with a horde of neuronal disorders such as PD, Read More..