Obesity affects many parameters that are otherwise normal in healthy individuals. Altered vitamin status is one such parameter. The article stresses upon how obesity and vitamin concentrations are linked.
Obesity is a mainly a consequence of consuming food rich in calories and poor in essential micronutrients. Such foods leave the body craving for the missing vitamins and minerals and trace elements, even if it is well fed with calories. Micronutrient deficiencies in obese people can affect leptin and insulin metabolism and could impair appetite regulation and energy metabolism in a myriad ways.
Besides inadequate intakes, micronutrient deficiency in obesity may also be due to altered metabolism.
Now, the question arises,
How to assess and define the optimal status of micronutrients in obese individuals?
There are some theories for it.
- Nutrient Deficiency Theory of Obesity
Nutrient deficiencies contribute to obesity because the body tells us to continue eating until all the micronutrient needs are met. This results in more calorie intake than needed. If this theory holds true, then getting a proper nourishment would aid in weight loss. However, the complication arises when a deficiency is an outcome of malabsorption and not inadequate dietary intake, in which case the cure for it isn’t necessarily consuming more of the nutrient in question.
- The Magical Supplement Theory of Obesity
As per this theory, if obesity is associated with deficiency of a particular nutrient, then megadose supplements of that nutrient must cause weight loss with no further effort required. Although much less plausible, the theory is widespread.
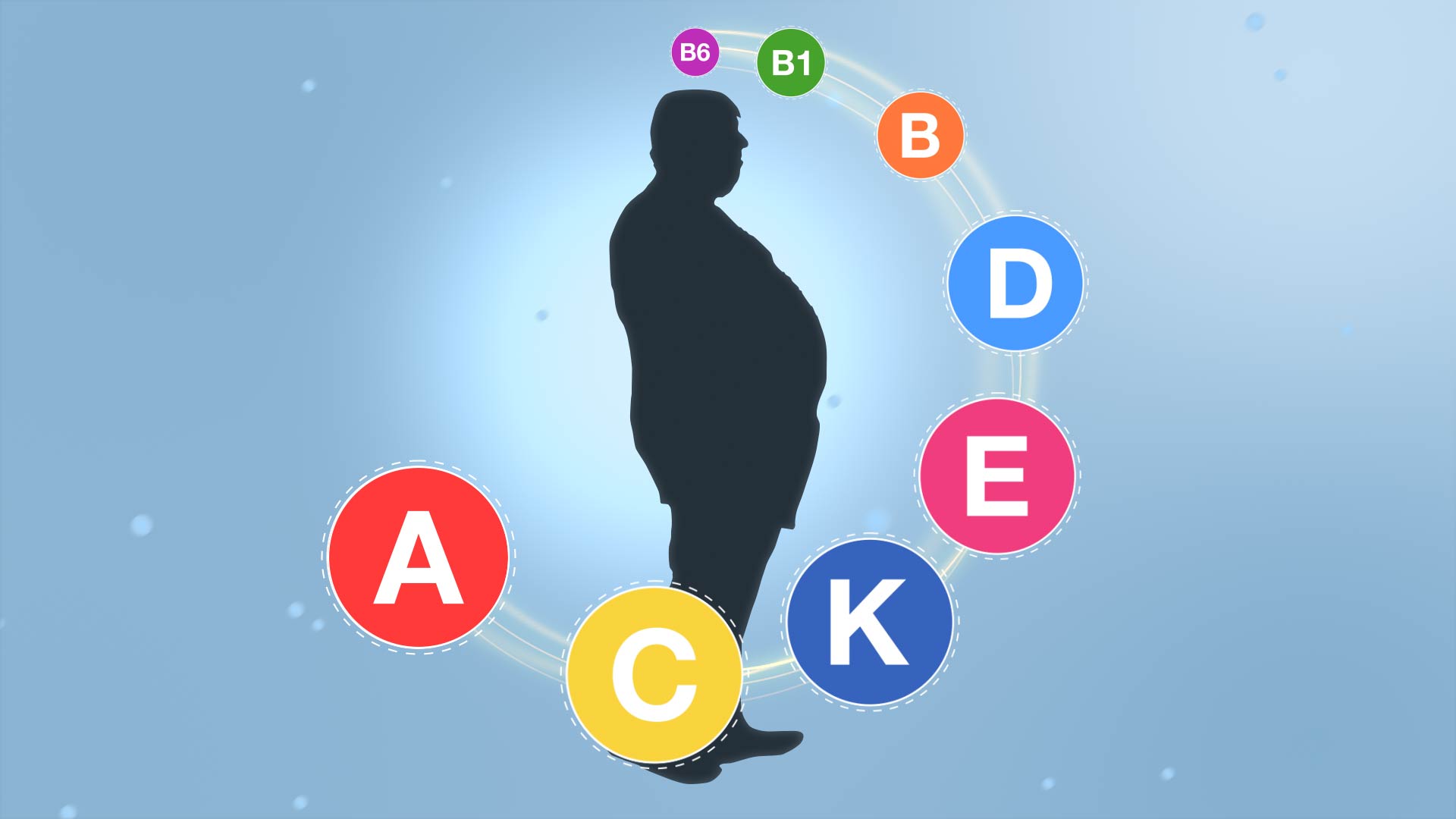
Vitamin status in obese individuals
Many research studies have observed the vitamin status of individuals suffering from metabolic syndrome (a group of conditions related to cardiovascular risk factors and obesity) in comparison to healthy individuals. Most of them have revealed that the levels of vitamin A, C and E are significantly lower in subjects when compared to healthy individuals. As concentrations of Vitamin A and C are associated with BMI, body fat and hormones that regulate fat deposition, it was concluded that decrease in these levels contribute to the weak antioxidative capacity in patients suffering from metabolic syndrome.
New research presented at the American Physiological Society (APS) annual meeting at Experimental Biology 2017 in Chicago suggests that normal levels of vitamin A within a high-fat diet can negatively affect expression of liver genes associated with glucose and fat metabolism.
High rates of vitamin D insufficiency have been reported in obese individuals and in diabetics. The prevalence of vitamin D insufficiency (defined as <30 mg/dL) in obese individuals ranges from 80–90%.
The link between obesity and vitamin D deficiency appears to be a one-way street. A large study of the genetics underpinning both conditions finds that obesity may drive down vitamin D levels, but a predisposition to the vitamin deficiency doesn’t lead to obesity. The findings also suggest that boosting vitamin D levels won’t reverse obesity. A meta-analysis says that the prevalence of vitamin D deficiency is 35% higher in people with obesity than in normal weight people. This is a cause of concern because vitamin D deficiency is a risk factor for heart disease, bone loss, impaired glucose metabolism causing diabetes, and all other kinds of chronic health problems associated with obesity.
Post the practice of vitamin fortification and witnessing aching rise prevalence of obesity globally, there is a pressing need to examine the relationship between vitamin fortification and vitamin paradox from the perspective of vitamin homeostasis.
Understanding the vitamin paradox in obesity and related diseases is crucial in determining how to manage the low vitamin status in these diseases. What is currently apparent is that the vitamin paradox in obesity may be due to increased vitamin degradation and storage to compensate the reduced vitamin excretion. This condition will continue until drug-metabolizing enzymes are saturated by their substrates, in which high expression of vitamin-degrading enzymes and elevated vitamin-metabolite levels may serve as indicators. The vitamin paradox can be resolved by reducing vitamin intake and increasing sweat rates, rather than by giving vitamin supplementation.
Given that there is a correlation between high vitamin intake and the increased prevalence of obesity, it can be assumed that obesity could be one of manifestations of chronic vitamin poisoning. It has been observed and reported that individuals prone to consuming excess vitamins are those with a low reserve capacity of excretory organs. Therefore, on an individual basis, prevention of obesity should focus on reducing their intake of vitamin-fortified foods, and for a country, more attention needs to be paid to the role of vitamin fortification and abuse in the increased prevalence of obesity and related diseases.
The explanation that reasons why being obese suppresses vitamin D is still debatable. Because of its fat soluble nature, some scientists had assumed that vitamin D got stored in fatty tissues, causing less of it to reach the bloodstream. However, there’s no strong evidence that fatty tissue sequesters and retains vitamin D.
As with nearly all biochemical processes, glucose metabolism and insulin signaling require cofactors and vitamins that are essential in the diet. Deficiencies in any of these micronutrients have potential to impair glucose metabolism and cause insulin resistance. Clinical evidence supporting this hypothesis regarding the metabolic effects of specific deficiencies including vitamin D, chromium, biotin, thiamine and vitamin C is mounting. Unlike vitamin E, which has little to no proven clinical effect when given as a supplement, these vitamins are known to be deficient at relatively high rates in obese individuals and in diabetic patients.
References:
- Vitamin paradox in obesity: Deficiency or excess?
- The Malnutrition of Obesity: Micronutrient Deficiencies That Promote Diabetes
- Link between obesity and vitamin D clarified
- Micronutrient deficiency in the aetiology of obesity

Squeezing Stomachs To Get Rid Of Obesity: An Account On Gastric Restriction
The epidemic of morbid obesity has paved way for a renewed interest in its surgical treatment. Bariatric surgery, proved to be associated with a significantly reduced number of cardiovascular deaths and a lower incidence of cardiovascular events in obese adults,Read More..








